Black and Hispanic children with AML tend to have worse outcomes compared to White non-Hispanic children. Potential contributing factors include higher acuity at presentation, higher infection related mortality, and less availability of hematopoietic stem cell donors (Winestone. Amer J Hematol. 2017; Aplenc. Blood 2006; Gramatges. PBC 2017). We hypothesized that differences in disease biology contribute to inferior outcomes along racial/ethnic lines, and these differences may be apparent among specific cytogenetic subsets.
To test this hypothesis, we mined the publicly available TARGET AML dataset which includes 956 newly diagnosed children with AML enrolled on Children's Cancer Group study CCG-2961 or Children's Oncology Group studies AAML03P1 or AAML0531. There were 557 White, non-Hispanic (WNH), 115 Black (including six Black Hispanic), 170 non-Black Hispanic, 45 Asian, and 69 patients of other races included in our analysis. Overall survival (OS) was defined as time from study entry until death; event free survival (EFS) was time from study entry to first event (induction failure, death, death without remission, or relapse). Patients were censored at the date of last contact. We used the Kaplan-Meier method to estimate OS and EFS; the log-rank statistic tested survival differences. Pearson's chi-squared or Fisher's exact test was used to test for differences between proportions. Welch's t-test, ANOVA, and Wilcoxon rank-sum tests were used for continuous variables.
Comparing tumor cytogenetics by race/ethnicity: when compared to WNH children, t(8;21) was more common among Black (OR=2.03; 95% CI: 1.20-3.42) and Hispanic (OR=2.04; 95% CI: 1.29-3.24) children. Black children were also more likely to have either -5/-5q or -7/-7q compared to WNH (OR=2.60; 95% CI: 1.29-5.23).
We then interrogated KMT2A rearrangements (KMT2Ar), finding that there was no difference in the percentage of patients with a KMT2Ar on the basis of race/ethnicity. The distribution of various KMT2A fusions in Hispanic patients was not significantly different than WNH, but Black children were more likely to have t(6;11)(q27;q23) both overall (OR=5.78; 95% CI: 1.73-19.28) and among patients with KMT2Ar (OR 7.29; 95% CI: 1.94-27.40). Black KMT2Ar children were older than WNH and Hispanic KMT2Ar children (11.2 vs. 6.5 years, p=0.002). Hispanic children with KMT2Ar had a higher presenting white blood cell count (WBC median 114,700/µL) compared to WNH (median WBC 49,600/µL; p=0.01) and Black (38,300/µL; p=0.006) children.
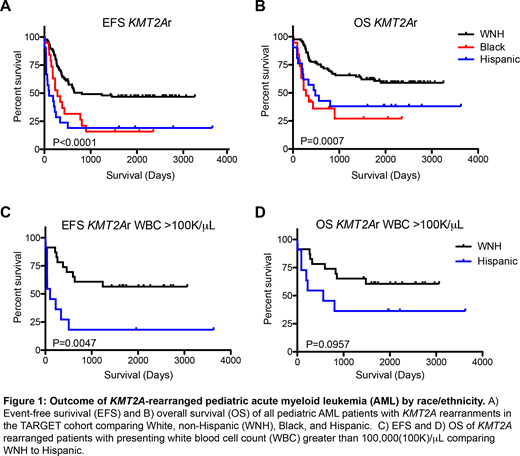
We then investigated survival: similar to prior studies, Black children had inferior EFS and OS compared to WNH (both p<0.0001). Hispanic and Asian children had similar survival to WNH children. However, the EFS/OS of both Black and Hispanic children with KMT2Ar were worse than WNH with KMT2Ar (Fig1A,B), though the reasons for poor outcome were different for Black and Hispanic children. Eight of 21 Hispanic children had induction failure compared to 0/19 Black and 1/85 WNH children (p<0.001), whereas Black children tended to suffer death or relapse as first event. Higher WBC at presentation did not explain the difference in outcome for Hispanic children: when we restricted our analysis to those with a presenting WBC >100,000/µL, Hispanic children still had an inferior EFS compared to WNH with a trend towards inferior OS (Fig 1C, D). The poor outcome of Black children with KMT2Ar may be driven by the higher proportion with the known poor prognostic t(6;11) and older age; but even when restricted to age >10yrs, Black children tended to have worse outcomes compared to WNH patients.
In conclusion, using the TARGET data set, we identified differences in tumor genetics, clinical features and outcome by race/ethnicity. Specifically, among KMT2Ar patients, we found that Black and Hispanic children had significantly worse outcomes than WNH - but for different reasons with potential biologic implications. The difference in age and distribution of KMT2A fusion among Black children suggest distinct AML pathogenesis, while higher presenting WBC and increased induction failure risk among Hispanic children suggest that genetic factors may contribute to disease phenotype and response to therapy. In ongoing work, we are investigating racial/ethnic differences in tumor biology and pharmacogenomics to better understand the causes of poor outcome with the ultimate aim of eliminating long-standing survival disparities.
Rau:Jazz Pharmaceuticals, Inc.: Consultancy, Other: Travel Fees.
Author notes
Asterisk with author names denotes non-ASH members.